The Psychiatric Interview / The Medical Interview
When interviewing any patient, whether in a psychiatric setting, or a
medical setting, the interviewer faces a number of options as to how best to
approach the interview, what the goals of the interview should be, how best to
maximize the finite and usually limited time available. There are as many
interview styles as there are interviewers and each style captures something
unique about the relationship between doctor and patient.
At each moment in the interview the interviewer faces a number of
opportunities and pitfalls, which can either deepen trust and understanding or
create greater difference and defensiveness. Probably the greatest mistake most
interviews make is asking too many too specific questions, turning the interview
into an interrogation.
In principle it is better to start with open-ended questions and follow
up on what the patient chooses to reveal about themselves. In practice this may
be more difficult than it seems. With practice, it becomes quite natural and
spontaneous.
All patients have a need to be understood and want to tell “their
story”. We might call this the “narrative imperative.” This is especially
manifested when someone comes to a doctor for help. But we need to appreciate
that most people do not know the kind of help they need, nor do doctors know
without listening carefully. There may be some dancing around the issues, or
back and forth volleying while the doctor tries to find out how forthcoming the
patient is prepared to be and the patient tries to find out how attentive the
doctor is prepared to be to their “inner self”. Even the most guarded paranoiac
wants to be understood.
It is thus tempting for the doctor to launch into a question and answer mode
when the patient initially hesitates. Communications specialists observing
doctor-patient interviews that this usually takes place in the first seconds of
an interview, not in minutes, and that even if patients start to elaborate their
concerns, doctors usually interrupt and direct the interview within the first
minute. Most medical interviewers are like the Joe Friday, the LAPD detective
of Dragnet fame: “Just the facts, Ma'me.” A more appropriate detective role
model might be Columbo, who though a bit rumpled, always listened patiently to
the story, then came back with follow-up questions.
The Minimal Activity Technique
The Minimal Activity Technique is a way of disciplining ourselves to let
the patient tell their story. It serves as a reminder that patients come to us
to talk and we can listen. We control the interview with a light touch. We
have two ears and one mouth for a reason and should probably use them in that
proportion.
The open-ended question: Recognizing that there is not one standard way
to interview patients, the interviewer should select an opening open-ended
question to start the interview. “Why have you come for help? “ “How can I
help you?” “Can you tell me something about yourself and your concerns?” “What
would you like to talk about today?” are all appropriate opening open-ended
questions.
Volleying or Dancing or Sparring: One may expect in the opening moments
of the interview the patient to clarify what is expected. Patients will often
ask, “What do you want to know?” which many doctors will take as a cue to
abandon the open-ended approach and launch into 40 questions and 40 answers.
This is a mistake. It reflects the doctors anxiety rather than confidence. It
is better to acknowledge the tension with another open-ended invitation.
“Whatever you feel is important?” or “Whatever you would feel most comfortable
talking about.” Often interviews will want to “make the patient feel
comfortable” by starting with chit-chat. This is also a mistake. An interview
that starts superficially usually stays superficially. If the doctor signals
that she or he is uncomfortable with feelings, the patient will pick up on
that. No one will feel comfortable talking about the humiliation of their
divorce or how hurt their were by childhood trauma right away, but they will be
testing the interviewer to see if this might be a place where they can feel
safe.
Stage One: Active listening. One the patient feels comfortable, the
interviewer can relax and listen to the patient’s narrative. Patients will
usually talk uninterrupted for many minutes if they feel they are being listened
to. The manic patient may talk forever and need to be interrupted. The
obsessive patient may give more details than we can initially make sense of,
and eventually need to be redirected, but listening precedes redirection.
Stage Two: Non-verbal encouragement. After the patient has been
talking for several minutes, they may stop or pause. This is not yet an
occasion to switch to the Q and A format? There will be a temptation to clarify
what the patient has said, but that is not necessary at this point. At this
point in the interview, it is better to encourage the patient to continue
talking and this can usually be done with a gesture like leaning forward,
looking at the patient directly and expectantly. The patient will usually
resume talking, and the interviewer can go back to active listening.
Stage Three: Verbal encouragement. After a period of active listening,
escalation to non-verbal encouragement perhaps several times, the patient may
pause again, uncertain about how to proceed. It is still not time to ask direct
questions. It may be more appropriate here to give some sort of verbal
encouragement: “Go on” “Is this difficult to talk about” “Can you say more
about that?” “What else?”
Caution: Stay with feelings. One of the biggest mistakes a medical
Joe Friday can make is to change the subject when patients begin to show
feelings, sadness especially but even anger or other feelings. . Patients will
be inclined to do this themselves. A supportive gesture, like offering a
tissue, is an acknowledgement of the feelings, but may suggest that tears should
be wiped away, so we can get on with fact-gathering. It may be better to ask,
“Can you put words on those feelings?” or at least to acknowlege in words what
you are observing: “This must be difficult to talk about.” or “You still have
feelings about this.”
Stage Four: Indirect question. After some time, the interviewer begins
to get some sense about how the patient is viewing their situation and is also
trying to make sense about what is being said. Indirect questions are
extensions of verbal encouragement and transitions to more direct questions.
Indirect questions facilitate the narrative by helping the patient begin to
observe what they are reporting. “You mentioned your mother, but haven’t said
anything about your father.” “How did you feel when you received the news?”
Stage Five: The Direct question. There are many options the
interviewer has before asking direct questions. By the time it is necessary to
ask direct questions, the patient will have told the doctor much of the needed
information, and the patient by tell his story in his way has also told the
doctor how they understand themselves and their situation. Although time has
been “lost” by letting the patient talk, much important information (and
understanding) has been gained. The direct questions that the doctor then asks
will be more meaningful for the patients and for the patience shown.
t=0 Establish rapport: Open –ended questions
Expect some volleying
Minimal activity technique
t=10 Think about Differential Diagnosis
t=15 Screening questions
t=20 Developmental history
t=25 Mental Status Questions pertinent to Diff Diagnosis
t=30 Feedback about what has been learned
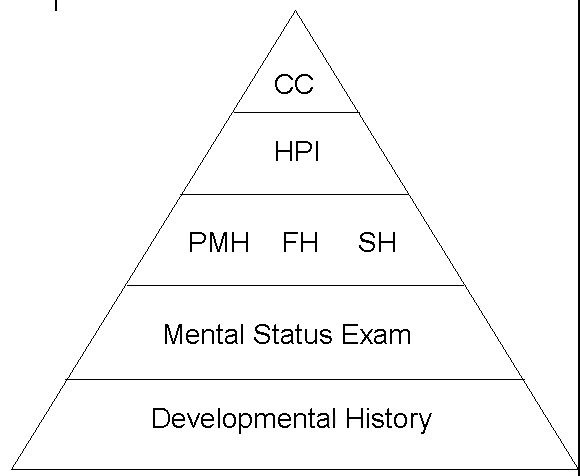
Building a History:
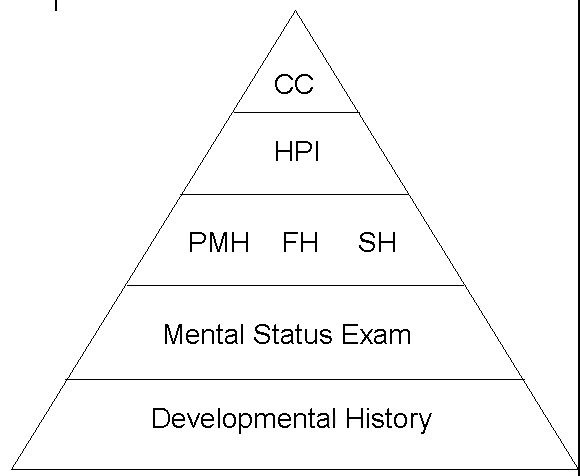
Building a History: By medical convention, the presentation of a history is in a certain border, starting with the chief concerns (not the chief complaint, please), progressing through the history of the present illness, the past medical history, the family history, social history, exams (physical exam, mental status exam, laboratory exams) and the Developmental History. Conceptually the Developmental Life History (or biography or patient narrative) is the foundation of the history we build with the patient. See more about the Developmental History and Repetition Compulsion.